Type 1 Diabetes Basics
Successful management of diabetes is as much about information as it is about insulin or oral medications.
Diabetes Basics is designed to supplement the information you receive from your medical team.
What is Type 1 Diabetes?
Type 1 diabetes is an autoimmune disease in which the body destroys insulin-producing beta cells in the pancreas. Insulin is required by the body to use glucose, the simple sugar that most foods are broken down into by our digestive system. Without insulin, the body starves to death. It’s important to note that everyone is insulin-dependent. People without diabetes make insulin in their pancreas. People with type 1 diabetes must inject insulin.
According to the National Institutes of Health, an estimated 850,000 to 1.7 million Americans have Type 1 diabetes. Of those, about 125,000 are kids 19 and under. An additional 30,000 Americans develop type 1 diabetes every year, 13,000 of whom are children. Type 2 diabetes is much more prevalent, with an estimated 16 million Americans having type 2. Millions of people with type 2 diabetes have not yet been diagnosed.
What Are the Symptoms of Type 1 Diabetes?
- Excessive thirst ( Polydipsia )
- Excessive urination ( Polyuria )
- Excessive hunger
- Weight loss
- Fatigue
- Blurred vision
- High blood sugar level
- Sugar and ketones in the urine
- Kussmaul breathing (rapid, deep, and labored breathing of people who have ketoacidosis or who are in a diabetic coma)
- Vaginal yeast infections in girls (even infants and toddlers)
- Bed wetting, especially when the child was not wetting previously
- Dehydration ( despite good fl uid intake )
- Vomiting
- Confusion
- Flu-like symptoms
- Fruity odor to breath
What Causes Type 1 Diabetes?
Diabetes develops gradually. Studies performed by the Joslin Clinic have shown changes as much as nine years before the actual presentation of diabetes symptoms. The development of type 1 diabetes can be broken down into five stages:
- Genetic predisposition
- Environmental trigger
- Active autoimmunity
- Progressive beta-cell destruction
- Presentation of the symptoms of type 1 diabetes
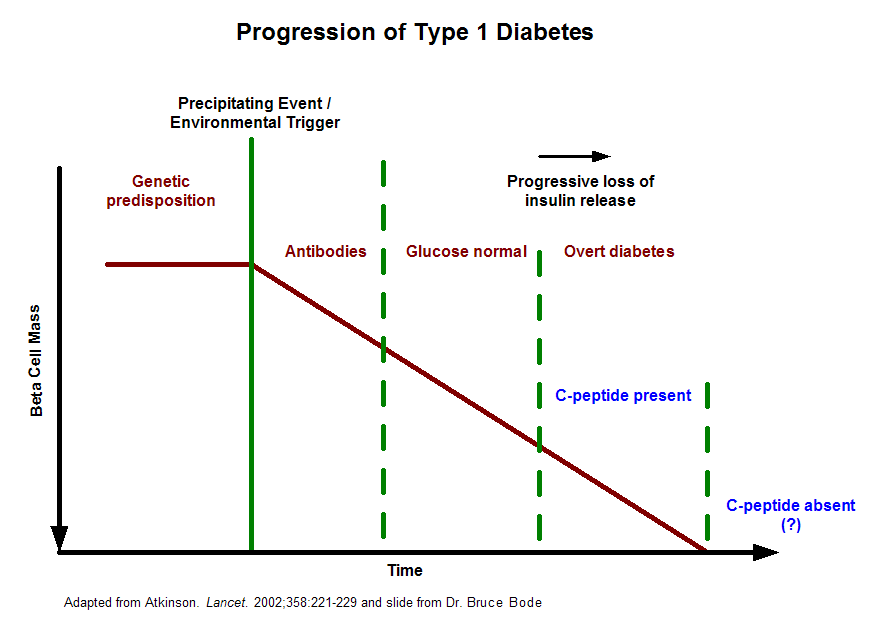
This graph illustrates the progression of islet mass loss that leads to overt type 1 diabetes. According to research by Dr. David Harlan of the NIH/NIDDK, some people with long standing type 1 diabetes have measurable c-peptide production, which may help reduce their risk of complications and could indicate that the body continues to generate new islets even in the face of the autoimmune attack of type 1 diabetes.
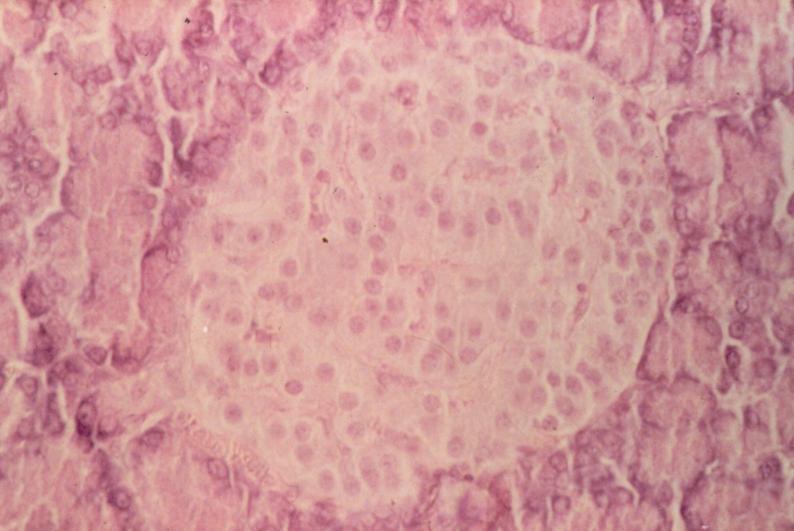
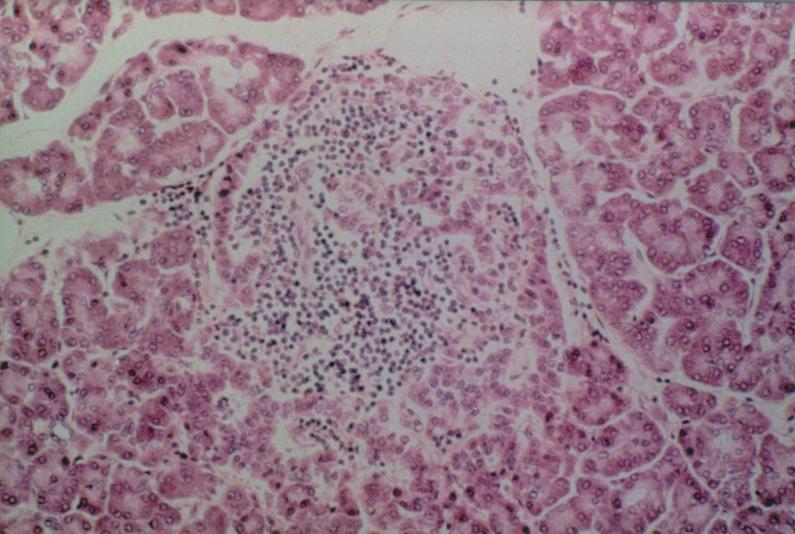
Type 1 Diabetes at the Islet Level
According to research, some people with long-standing type 1 diabetes have measurable c-peptide production, which may help reduce their risk of complications and could indicate that the body continues to generate new islets even in the face of the autoimmune attack of type 1 diabetes.
People with type 1 diabetes have a genetic pre-disposition to the disease, but one or more environmental insults is required to trigger disease. This fact can be derived from studies of identical twins with type 1 diabetes. When one twin has type 1 diabetes, the other twin gets diabetes only half the time. If the cause of type 1 diabetes were purely genetic, both identical twins would always have type 1 diabetes.
One environmental trigger is thought to be the Coxsackie B virus. Researchers at UCLA found that a small segment of GAD is structurally similar to a segment of a Coxsackie B protein. GAD is found on the surface of insulin-producing beta cells. The implication is that the body’s immune system, after warding off the Coxsackie B virus, continues to attack beta cells because of the similarity of GAD to the virus.
The environmental trigger results in the production of autoantibodies. People with type 1 diabetes have antibodies in their blood that indicate an “allergy to self,” or an autoimmune condition. One autoantibody found in people with type 1 diabetes is the islet cell antibody. This antibody is often present months or years before the diabetes presents. Other antibodies include the GAD (or 64-K) antibody and the ICA 512 antibody. The presence of these antibodies is a sign that the body is attacking its own beta cells.
What Are the Risks of Developing T1 Diabetes?
The overall incidence of autoimmune or type 1A Diabetes in the U.S. and Western Europe is approximately 0.4% in Caucasian families in the first 20 years of life. The figure varies with its geographical distribution, being significantly higher in Finland and lower in Scotland. The incidence is lower in Asian, African American and Hispanic families and also appears to be increasing slowly.
In families where there is already a first degree relative with this form of diabetes, the chances of a future or so far unaffected child developing this condition is about 5%; slightly higher if the father is affected and slightly lower if it is the mother.
In individual cases the risk to a so far unaffected child can be further refined by establishing the HLA distribution on chromosome 6, with special regard to the presence of high risk and protective patterns. To date there are no certain estimates for the impact of environmental factors.
Treatment for Diabetes
Type 1 diabetes is treated with daily injections of insulin. Oral diabetes medications are not effective. Many patients with type 1 diabetes, after beginning insulin injections, experience a period of reduced insulin need called the honeymoon period. During the honeymoon period, the remaining beta cells continue to produce insulin. It is very important to continue insulin therapy during the honeymoon period, because even low doses of insulin appear to help prolong the duration of the honeymoon.
Treatment for type 1 diabetes includes:
1. Taking insulin
2. Carbohydrate, fat and protein counting
3. Frequent blood sugar monitoring
4. Eating healthy foods
5. Exercising regularly and maintaining a healthy weight
There are currently several tools available to help track and maintain blood sugar levels, including insulin pumps, smart pens, CGMs (Continuous Glucose Monitoring Systems), and blood glucose meters.
What is insulin?
Insulin is a hormone produced by beta cells in the pancreas. It has three important functions:
- Insulin allow glucose to pass into cells, where it is used for energy.
- Insulin suppresses excess production of sugar in the liver and muscles.
- Insulin suppresses the breakdown of fat for energy.
In the absence of insulin, blood sugar levels rise because muscle and fat cells aren’t able to utilize glucose for energy. They signal the body that they’re “hungry.” The liver then releases glycogen, a form of stored glucose. This further increases the blood sugar level. When the blood sugar level reaches about 180 mg/dl, glucose begins to spill into the urine. Large amounts of water are needed to dissolve the excess sugar, resulting in excessive thirst and urination.
Without glucose for energy, the body begins to metabolize protein and fat. Fat metabolism results in the production of ketones in the liver. Ketones are excreted in the urine along with sodium bicarbonate, which results in a decrease in the pH of the blood. This condition is called acidosis. To correct the acidosis, the body begins a deep, labored respiration, called Kussmaul’s respiration. Left unchecked, a person in this situation will fall into a coma and die.

Why Does It Have to Be Injected?
Insulin must be injected because it is a protein. If it were taken orally, the body’s digestive system would break it down, rendering it useless.
One type of insulin (Afrezza) is inhaled instead of injected.
Where Should I Store It?
Unopened insulin vials should be kept cool. Storing them in the refrigerator will help them last as long as possible. Never freeze insulin, however, as freezing can destroy it. Open insulin, whether vials or pens, can be kept at room temperature for about a month.
Where Does Insulin Come From?
Insulin used by people with diabetes can come from three sources: human (created via recombinant DNA methods), pork, or beef. Beef insulin has been discontinued in the US, and essentially all people who are newly diagnosed are placed on human insulin.
Find out more about insulin, including what kinds are available and information on administering it:
- The Beginner’s Guide to Diabetes by the Joslin Diabetes Center offers a good introduction to diabetes.
- Diabetes Overview from the National Institutes of Health
- Type 1 Diabetes: Cellular, Molecular & Clinical Immunology from the Barbara Davis Center for Diabetes
- Understanding Insulin-Dependent Diabetes by H. Peter Chase, M.D.
- Management of Diabetes Mellitus: Perspectives of Care Across the Life Span edited by Debra Haire-Joshu, MSEd, MSN, PhD, RN
- Srikanta S and others: “Islet-cell antibodies and beta-cell function in monozygotic triplets and twins initially discordant for type I diabetes,” New England Journal of Medicine, 308:322-325, 1983.
- Common Class of Viruses Implicated as Cause of Type 1 Diabetes and Getting the Goods on GA
- Challenges in diagnosing type 1 diabetes in different populations. Free full text available in HTML and PDF formats.
- Type 1 diabetes and latent autoimmune diabetes in adults (LADA): one end of the rainbow. Free full text available in PDF format.
- After Rotavirus Vaccine, Australia’s Type 1 Diabetes Incidence Declines. Free full text available in HTML.